WHAT IS DIABETES?
Diabetes is a chronic health condition that affects how your body turns food into energy. When the food you eat is broken down into sugar (also called glucose) and released into your bloodstream, your blood sugar goes up. This signals your pancreas to release insulin, which lets blood sugar into your body’s cells to use as energy. If you have Diabetes, your body does not make enough insulin or cannot use insulin as well as it should. When this occurs, too much blood sugar stays in your bloodstream. Over time, this can cause serious health problems, such as heart disease, vision loss, and kidney disease. There is no cure yet, but taking medication, getting diabetes self-management education and support, and improving lifestyle habits can reduce the impact of Diabetes on your life.
TYPES OF DIABETES
Type 1
This is caused by an autoimmune reaction (when the body attacks itself by mistake) that stops your body from making insulin. Approximately 5-10% of people with diabetes have Type 1. In this case, symptoms develop quickly. It is usually diagnosed in children, teens and young adults. If you have this type, you will need to take insulin every day for survival. Currently, there are no ways to prevent Type 1 diabetes. Risk factors include:
- Family history: having a parent or sibling with type 1 diabetes.
- Age: more likely to develop when you are a child, teen, or young adult.
- Race/ethnicity: Caucasian
Type 2
In this case, your body does not use insulin as well as it should and cannot keep blood sugar at normal levels. About 90-95% of people with diabetes have Type 2. It develops overtime and is usually diagnosed in adults. However, in recent years more cases are being seen in children and adolescents. Type 2 diabetes can be prevented or delayed with healthy lifestyle changes. This may include losing weight, eating nutritious food, and increasing physical activity levels. Risk factors include:
- Have pre-diabetes
- Weight status: Overweight
- Age: 45 years or older
- Family history: have a parent or sibling with type 2 diabetes
- Physically active less than 3 times per week
- Have had gestational diabetes or given birth to a baby that weighed more than 9 lbs.
- Race/ethnicity: African American, Hispanic/Latino American, American Indian, or Alaska Native.
Prediabetes
Blood sugar levels are higher than normal, but not high enough yet to be diagnosed with type 2 diabetes. This may raise your risk for type 2 diabetes, heart disease, and stroke. In the United States, 88 million adults (1 in 3) have prediabetes. Risk factors include:
- Weight status: overweight
- Age: 45 years or older
- Family history: have a parent or sibling with type 2 diabetes
- Physically active less than 3 times per week.
- Have had gestational diabetes or given birth to a baby that weighed more than 9 lbs.
- Race/ethnicity: African American, Hispanic/Latino American, American Indian, or Alaska Native.
Gestational
This develops in pregnant women who have never had diabetes. This can put your baby at a higher risk for health problems. This type of diabetes usually goes away after your baby is born but can increase your risk for type 2 diabetes later in life. This can also increase the risk of your baby experiencing obesity or type 2 diabetes later in life. Risk factors include:
- Had gestational diabetes during a previous pregnancy.
- Have given birth to a baby that weighed more than 9 lbs.
- Weight status: overweight
- Age: 25 years or older
- Family history: parent or sibling with type 2 diabetes or gestational diabetes
- Have polycystic ovarian syndrome (PCOS)
- Race/ethnicity: African American, Hispanic/Latino American, American Indian, Alaska Native, Native Hawaiian, or Pacific Islander.
MANAGING DIABETES
Carb Counting
Counting carbohydrates can help you match your activity level and medicines to the food you eat. Many people count carbs to make managing blood sugar easier, which can assist with overall health, improving quality of life, and preventing or delaying complications. If you take mealtime insulin, you will count carbs to match your insulin dose to the amount of carbs in your food and drinks. Furthermore, you may also take additional insulin if your blood sugar is higher than your target when eating.
On average, people with diabetes should aim to get about half of their calories from carbs. These are measured in grams. For diabetes meal planning, 1 carb serving is about 15 grams of carbs.
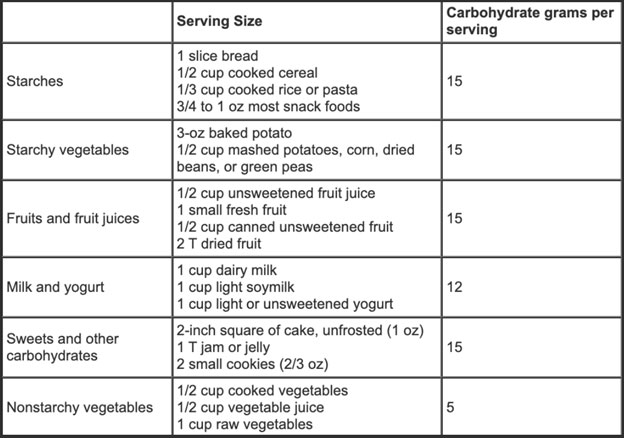
Carbohydrate Foods, Serving Sizes, and Carbohydrate Grams Per Serving
Sample Meal Plan Based on 2000 kcal/day
Breakfast: 1/2 c oatmeal + 2 tbsp raisins + 1/4 cup pecans
Snack: apple + 2 tbsp peanut butter + 1 oz pretzels
Lunch: 1 c brown rice + 1/2 c cooked vegetables + 3 oz grilled chicken
Dinner: 1 c whole wheat pasta + 1/2 c cooked vegetables + 3 oz salmon
Snack: 1 bagel + 2 tbsp cream cheese
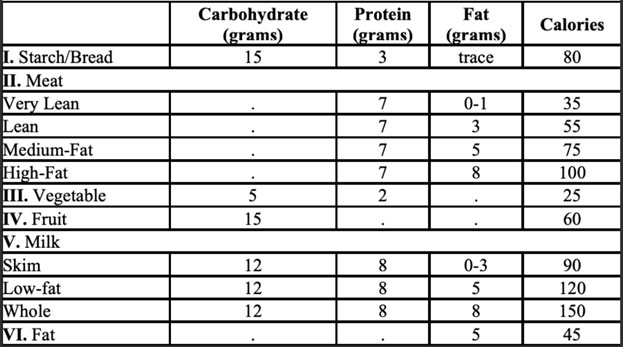
Diabetic Exchange List
The exchange lists are broken into 6 food groups. Foods are grouped together because they are alike. Foods on each list have about the same amount of carbohydrate, protein, fat and calories. In the amounts that are given, all choices on each list are equal. Any food on the list can be exchanged or traded for any other food on the list. The following chart shows the amounts of nutrients in one serving from each exchange list:










Get Social